Dr. Ronald Perkins discusses symptoms of sleep disorders and his treatment protocol
 An as an orthodontist since the early 1970s, I typically recommended the surgical removal of the enlarged tonsils and adenoids that caused airway blockage in young children. The results of this well-known surgical procedure were immediate: Parents reported that their children were sleeping more restfully, with no snoring and were much easier to wake up in the morning. Within a few months, parents would often say that their children’s schoolwork was improving, along with their health and attitude.
An as an orthodontist since the early 1970s, I typically recommended the surgical removal of the enlarged tonsils and adenoids that caused airway blockage in young children. The results of this well-known surgical procedure were immediate: Parents reported that their children were sleeping more restfully, with no snoring and were much easier to wake up in the morning. Within a few months, parents would often say that their children’s schoolwork was improving, along with their health and attitude.
[userloggedin]
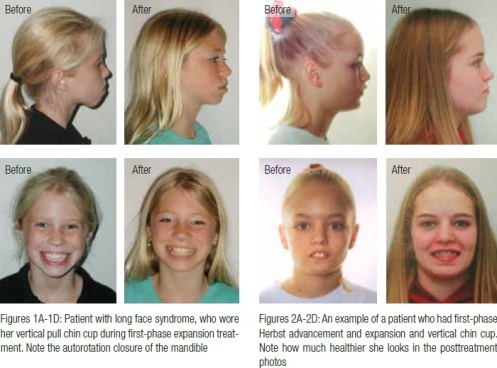
After studying the work of Dr. Rolf Frankel and others,1,2,3 who speculated that form followed function and that mouth breathing could affect growth in children, especially regarding long face syndrome and the use of a vertical-pull chin cup therapy, I started using this therapy, along with the removal of tonsils and adenoids, palatal expansion, and mandibular advancement. The pre- and posttreatment photos (Figures 1A-1D and 2A-2D) show the results: healthy children with the reduction and correction of this vertical growth problem.
Firsthand observations of sleep disorder symptoms
As an orthodontist, I was aware of pediatric airway problems and sleep disorders but unaware of my own sleep disorder. I suffered with weight gain, fatigue, and loud snoring. Fortunately, an alert physician heard me fall asleep in his exam room and recommended that I get a sleep study. Soon after, I encountered an old friend from dental school, Dr. Keith Thornton, inventor of the TAP® (Thornton Adjustable Positioner) appliance at a dental event, and he recognized my sleep disorder too. Within 2 weeks, I was fitted with the oral appliance.
My first night of sleep in the TAP appliance was an epiphany. Normally, I would hit the snooze button at least 2 times before I could get out of bed. But on this night, for the first time in my adult life, I woke up refreshed before the alarm sounded, without fibro-myalgia, numb feet, or acid reflux. I also woke up in the same position and did not “tear up the bed” with my restless sleep. During the day, I was much more energetic. I now recognized a few of the many symptoms of sleep disorders.4,5,6 In the next few months, I lost approximately 40 pounds because I was burning more calories during my sleep, and I felt more like exercising. I began to record the changes after recognizing the symptoms that were improving in my life.
In the meantime, the oral appliance was working well, but my jaw joints were uncomfortable in the morning, so I decided to balance my own appliance to support the joints during sleep, which made me feel even better. Unfortunately, I waited a little too long to balance my appliance because I had developed a Class III occlusion, an all too common side effect of oral appliances. (This bite change is probably the main reason many dentists are reluctant to treat patients with oral appliances.)
Because my balanced oral appliance was so much more comfortable, I decided to treat all my patients who wore this in the same manner. The results seemed phenomenal, with very few side effects and without creating Class III occlusions. Across the board, I observed a reduction of my patients’ symptoms, as well as a reduction of their headaches. From 30 years’ experience and training in treating temporomandibular joint (TMJ) problems mostly with splints, I became more convinced of the effectiveness of this type of comprehensive treatment. In the past, I was really treating one of the major symptoms of sleep disorders, not the real cause, which is often the nightly clenching and bruxing that adversely affects the jaw joints. Now my goal is to treat the sleep disorder and the TMJ problems at the same time.
This drastic improvement in my life and near-death experience (I was holding my breath for a full minute and having oxygen desaturation of at least 50%), spurred me to start helping others with sleep disorders. I began to recognize their symptoms, which were similar to mine. Along with reading the most current research in sleep medicine, I started to develop a comprehensive list of symptoms to evaluate and treat patients with potential sleep disorders. Many adult patients were referred to me for TMJ problems, and I began to recognize that many of those patients had symptoms of sleep disorders.7
How do oral sleep appliances work?
Even though there are many different types of appliances, the most commonly used mandibular advancement device (MAD) appliances, such as the TAP, work by slightly advancing the mandible and the tongue to a position forward enough to hold the airway open when the throat muscles relax, thereby preventing airway collapse during deep sleep. My preference from clinical experience is that these appliances should be custom-balanced to support the jaw joints during sleep so as to reduce side effects, such as headaches and bite change. In my practice, the TMJ-balanced TAP appliance and the AM Aligner are used for preventing unwanted bite changes. At the appliance delivery appointment, the AM Aligner (a low-heat ThermAcryl® wafer) is easily formed in the patient’s mouth to his/her normal occlusion or bite. The patient must use this bite wafer or AM Aligner every morning, usually for 10 to 15 minutes, to slowly and gently reposition the jaw back to the normal position (Figure 3).
Symptoms of sleep disorders
The symptom list in Table 1 helps to detail the patient’s progress. For example, if the patient is no longer snoring, waking up more refreshed, having no acid reflux, and no morning headaches, this illustrates that the appliance is working. I will also check for any joint symptoms and adjust the appliance as necessary.
Oral and facial symptoms, such as dark circles or bags under the patients’ eyes, also signal sleep disorders. An interview using the in-depth initial symptom list (Table 1) usually reveals many more symptoms.
 Each patient is unique with his/her own particular set of symptoms. (I highly recommend my patients read an outstanding book called Sleep Interrupted by Steven Y. Park, MD, to help them understand their symptoms.) From my experience, many of the adult patients I interview are able to trace these sleep problems to their childhood. The August 2012 edition of Pediatrics®, the official journal of the American Academy of Pediatrics, reported current clinical guidelines regarding childhood sleep disorders. In my opinion, orthodontists could play a very important role, in collaboration with pediatricians and sleep physicians in helping young children with these problems using early orthopedic treatment.
Each patient is unique with his/her own particular set of symptoms. (I highly recommend my patients read an outstanding book called Sleep Interrupted by Steven Y. Park, MD, to help them understand their symptoms.) From my experience, many of the adult patients I interview are able to trace these sleep problems to their childhood. The August 2012 edition of Pediatrics®, the official journal of the American Academy of Pediatrics, reported current clinical guidelines regarding childhood sleep disorders. In my opinion, orthodontists could play a very important role, in collaboration with pediatricians and sleep physicians in helping young children with these problems using early orthopedic treatment.
Children can have slightly different symptoms than adults (Tables 2 and 3). Snoring in a child is a possible sign of airway obstruction. Consider these questions: Is the child a restless sleeper? Is the child often tired and/or cranky? Dark circles under a child’s eyes, or “allergic shiners,” may be a sign of sleep deprivation, just as in adults. Large tonsils, retrusive jaws, narrow or constricted dental arches, bad dreams, and bed-wetting may all point to sleep disorders as well.
and 3). Snoring in a child is a possible sign of airway obstruction. Consider these questions: Is the child a restless sleeper? Is the child often tired and/or cranky? Dark circles under a child’s eyes, or “allergic shiners,” may be a sign of sleep deprivation, just as in adults. Large tonsils, retrusive jaws, narrow or constricted dental arches, bad dreams, and bed-wetting may all point to sleep disorders as well.
The oral exam
A simple oral dental exam can begin to show the clinician signs of bruxism, obstruction, and snoring. The oral exam should include checking for extremely heavy bone formation around the teeth, including tori and exostosis in many cases — a sign that patients may have been bruxing or clenching for a long time, perhaps since childhood. Teeth obviously worn from bruxing and numerous crowns in older adults are also apparent signs in many patients. The next step is to look beyond the teeth into the posterior palatal areas and look for inflammation of the soft palate and uvula, possibly due to snoring or obstruction. There can also be inflammation of the oral pharynx due to acid reflux (see Figure 4). The size of the airway — small, medium, or large (Mallampati scores) — is also a determining factor. Tonsils should not be large enough to obstruct the airway. The next step is the palpation of the muscles of mastication and TMJ areas to determine if the patient is clenching regularly or has pain coming from either jaw joint. Pressing orally behind the retromolar area will elicit severe pain in patients whose muscles are tense from bruxing or clenching, and many of these patients will have headaches behind their eyes. Next, using the stethoscope, I listen to the joints and evaluate crepitus and popping. From my clinical experience, patients with medial pops and the history of locking seem more likely to have problems with an oral appliance.
After discussing the exam results with patients (who have obvious symptoms) and the benefits to their health of treating their sleep disorder, I would then request a sleep study, evaluated by a sleep physician, who will then make recommendations for treatment. Patients can choose between a home study or an overnight study in a clinic. State laws vary from state to state with regard to the dentist’s role in treatment and diagnosis of sleep disorders, so always be aware of your particular state’s practice rules and regulations.
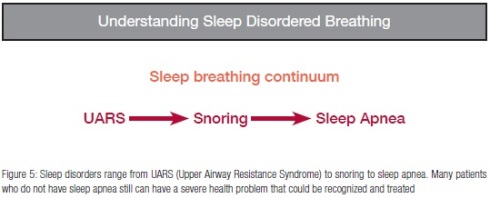
Upper Airway Resistance Syndrome (UARS) is the first level of a continuum of sleep disorders (Figure 5) that starts with UARS and progresses through snoring, on to severe apnea.9,10,13 Many patients who snore or have UARS9,10,13 can be treated with a dental appliance. I see many patients with UARS who are just as miserable and sleep deprived as patients with severe apnea. The patients who have UARS just stop breathing enough to cause awakening, which disrupts the sleep cycle, causing clenching and bruxing of the teeth. Another typical symptom of patients is forgetting their dreams, or having no dreams or bad dreams. With treatment, many patients start having memorable, vivid dreams — another positive treatment result for many patients, especially young adults and children.
 If patients are ready to start, we will take routine diagnostic records (X-rays, photos, and appliance impressions). As a part of these diagnostic records, the standard cephalometric X-ray also allows for a good view of the adenoid tissue in the upper airway, especially in children. My goal is to teach patients to monitor their sleep disorder by understanding their symptoms. I ask adult patients to record both their evening blood pressure and morning blood pressure for at least 3 days and bring that written record to their next appointment. In many cases, the patients with high blood pressure will often see a lowering of their pressure with treatment, especially in the morning. I have seen patients lowering blood pressure 10 points the first night they used their appliance, a good sign that treatment is working. Another telling symptom is the tendency to jump or jerk when falling asleep. This often can be the first time the patient obstructs or snores, and they are immediately awakened. Patients’ feedback indicates that wearing the appliance promotes more restful sleep with much less insomnia (also a revealing symptom).
If patients are ready to start, we will take routine diagnostic records (X-rays, photos, and appliance impressions). As a part of these diagnostic records, the standard cephalometric X-ray also allows for a good view of the adenoid tissue in the upper airway, especially in children. My goal is to teach patients to monitor their sleep disorder by understanding their symptoms. I ask adult patients to record both their evening blood pressure and morning blood pressure for at least 3 days and bring that written record to their next appointment. In many cases, the patients with high blood pressure will often see a lowering of their pressure with treatment, especially in the morning. I have seen patients lowering blood pressure 10 points the first night they used their appliance, a good sign that treatment is working. Another telling symptom is the tendency to jump or jerk when falling asleep. This often can be the first time the patient obstructs or snores, and they are immediately awakened. Patients’ feedback indicates that wearing the appliance promotes more restful sleep with much less insomnia (also a revealing symptom).
Orthopedic/orthodontic treatment for young children needing airway development
Now, as I look back at the many patients treated with the Herbst mandibular advancement appliance or with palatal expansion, also including mandibular uprighting expansion to enlarge the developing dental arches to create more tongue space, I realize that their improved health resulted from treatment similar to that of sleep disorders. Most children facially appeared so much healthier, and 20 years ago, I did not understand why this was such a common result. Orthopedic changes were creating more tongue space, as well as allowing the tongue to posture forward, just like an oral sleep appliance. I recognize now that advancing the mandible with the Herbst device has helped many young children breathe better at night. The parents have reported the dramatic results similar to those often seen with removal of tonsils and adenoids.
Along with expansion and mandibular advancement, in most of my patients who will cooperate, I use a vertical-pull chin cup not only to modify vertical growth but also to help the growing child use his/her airway. Parents are very supportive when they understand what these appliances can do for their child’s long-term health. I learned early from several ENTs that if a person does not use his/her nose, the tissues will expand from this non-use. Therefore, in growing children, why not help them breathe through their nose and develop the upper airway?
Orthodontists could perform a major role in helping to prevent or reduce the incidence of sleep disorders with progressive early treatment by expanding arches and advancing mandibles or maxillas in some cases and increasing the airway. In my practice, the experience of treating patients with sleep disorders has greatly increased the importance of non-extraction treatment to create tongue space, which can best be accomplished when the child is young (7 or 8 years old). This could be the only time we can truly expand the airway and help the patients sleep better the rest of their lives.
Cases in point
Another important fact to keep in mind when evaluating symptoms is that sleep disorders seem to run in families. In other words, as an orthodontist treating all age groups and families, I have seen a strong correlation of multiple family members having sleep problems.15 Often, the parents would tell me that they had the same problems as a child that their offspring was experiencing. For example, an 18-year-old previous patient returned because of a broken retainer; 4 years after I had completed his treatment, I noticed he was very tired, and after questioning him, I found he had numerous symptoms of a sleep disorder. I called his father, who I had treated for a sleep disorder 9 years earlier, to discuss his son’s issue. The father disclosed that the son had been involved in four automobile accidents, and he had fallen asleep while driving. Before I could get him into a sleep appliance, he had another wreck. It is important to be aware of patients who are tired and cranky, yawn a lot, and always look tired during their orthodontic treatment. You might just help save a young teenager’s life.
Recognizing and treating patients with sleep disorders has truly been the most rewarding experience of my life. Being an orthodontist, which I have always loved, involves treating our patients often for 2 years or more to achieve that final result when the appliances are removed and the patient is really happy. When treating adult patients with sleep disorders, I often have patients return to my office in 1 week commenting, “This appliance has changed my life,” and they often have new attitudes. Young mothers will often comment that they now have the energy to keep up with their children. If orthodontists can prevent a few more children from developing ADD, ADHD, and other cognitive problems by getting more oxygen to their developing brains,11,12,13 we can really make a difference and improve the quality of life for many people.
References
1. Moss ML, Rankow RM. The role of the functional matrix in mandibular growth. Angle Orthod.1968;38(2):95-103.
2. Frankel R. The functional matrix and its practical Importance in orthodontics”. Rep Congr Eur Orthod Soc. 1969:207-218.
3. Harvold EP. The role of function in the etiology and treatment of malocclusion. Am J Orthod. 1968;54(12):883-898.
4. Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Owens J, Pancer JP. Practice Parameters for the Treatment of Snoring and Sleep Apnea with Oral Appliances: An Update for 2005 [Report]. The American Academy of Sleep Medicine. SLEEP. 2006;29(2):240-243.
5. Beninati W, Harris CD; Herold DL; Shepard JW Jr. The effect of snoring and obstructing sleep apnea on the sleep quality of bed partners. Mayo Clin Proc. 1999;74(10):955-958.
6. Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, FJ Nieto, GT O’Connor, LL Boland, JE Schwartz, JM Samet. Sleep disordered breathing and cardiovascular disease: cross sectional results of the sleep heart health study. American Journal of Respiratory and Critical Care Medicine. 2001;163(1):19-25.
7. Colten HR, Altevogt BM, eds. Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC): National Academies Press (US); 2006. The National Academies Collection: Reports funded by National Institutes of Health.
8. Marcus CL, Brooks LJ, Draper KA, Gozal D, Halbower AC, Jones J, Schechter MS, Ward SD, Sheldon SH, Shiffman, RN, Lehmann C, Spruyt K. Diagnosis and management of childhood obstructive apnea syndrome. Pediatrics. 2012;130(3):e714-755.
9. Guilleminault C, Stoohs R, Clerk A, Cetel M, Maistros P. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest. 1993;104(3):781-7.
10. Bao G, Guilleminault C. Upper airway resistance syndrome — one decade later. Curr Opin Pulm Med; 2004;10(6): 461-467.
11. Huang YS, Guilleminault C, Li HY, Yang CM, Wu YY, Chen NH. AttentionDeficit/Hyperactivity Disorder with Obstructive Sleep Apnea: A Treatment Outcome Study. Sleep Med. 2007;8(1):18-30.
12. Gottlieb DJ, Vezina RM, Chase C, Lesko SM, Heeren TC, Weese-Mayer DE, Auerbach SH, Corwin MJ. Symtoms of sleep-disordered breathing in 5 year-old children are associated with sleepiness and problem behaviors. Pediatrics. 2003:112(4):870-877.
13. Park SY. Sleep Interrupted. New York: Jodev Press; 2008.
14. Gilles L, Cistulli P, Smith M. Sleep Medicine for Dentists: A Practical Overview. Illinois: Quintessence Books; 2009.
15. Casale M, Pappacena M, Rinaldi V, Bressi F, Baptista P, Salvinelli F. Obstructive Sleep Apnea Syndrome: From Phenotype to Genetic Basis. Curr Genomics. 2009;10(2):119–126.
[/userloggedin]
[userloggedout][/userloggedout]
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores



