CEU (Continuing Education Unit): 2 Credits
Educational aims and objectives
This self-instructional course for dentists aims to ensure better long-term outcomes for oral and whole-body health through proper breathing.
Expected outcomes
Orthodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize signs of oral breathing in adults and children.
- Realize consequences of untreated mouth breathing for dental health.
- Identify why surgery often fails to resolve oral breathing.
- Identify steps to restore nasal breathing during wakefulness and sleep.

Patrick McKeown discusses simple breathing re-education techniques for children and adults for oral and whole-body health
Most dentists, regardless of experience, understand the dangers of oral breathing.1 Yet there is currently no standardized procedure for dentists to identify mouth breathing in their pediatric or adult patients. Moreover, a vital step is missing in the long-term treatment of nasal obstruction. Patients with oral breathing are left frustrated as they experience bad breath, tooth decay, and malocclusion, despite careful brushing. Toothbrush use is the most important measure for oral hygiene.2 However, when patients breathe through the mouth for part of the day or night, even the most meticulous brushing cannot prevent problems.
In a 2019 letter to the American Dental Association, dentists, including Drs. Kevin Boyd and Steve Carstensen, urged awareness, stating: “Our young patients’ health is connected to their ability to take every breath through their noses, keep their mouths closed, and shape the growing craniofacial respiratory complex by proper tongue placement during swallowing.”3
It’s time to connect the dots and add simple breathing re-education techniques to the dental tool kit — to ensure better long-term outcomes for oral and whole-body health.
Mouth breathing in children and adults … has major implications for craniofacial development in children, and it contributes to gum disease, dental cavities, and bad breath — all problems the dentist works to resolve.
Oral breathing: how big is the problem?
The prevalence of mouth breathing is understudied, but the figures we do have are significant. One 2020 study reported that 17.2% of patients aged 3 to 83 years primarily breathed through an open mouth.4 Previous research in children identified that about 55% were mouth breathers.5,6 A recent cross-sectional study of children aged between 6 and 12 years found that 51% were “mixed breathers,” meaning they breathed through the mouth at least some of the time.7
There is increasing evidence that oral breathing contributes to dental conditions such as gum disease, halitosis, and cavities. There’s a serious cost to overall well-being too.
Mouth breathing: more than just a dry mouth
When saliva dries up due to mouth breathing, the acidity of the mouth increases. Acid-producing bacteria thrive, and the buffering capacity of saliva is compromised. This contributes to plaque and tartar buildup,8 oral thrush,9 and mineral loss10 from the surface of the teeth leads to dental caries. Studies in children have shown statistically significant correlations between mouth breathing and halitosis.11 In adults, dry mouth, is linked with obesity, arterial hypertension, and hyperglycemia.12
It’s important to note that mouth breathing does not need to be constant for problems to occur. The researchers in one study refer to mixed oronasal breathing as “one of the most deleterious habits” in terms of malocclusion.7 Another study reports that when increased separation of the lips or decreased upper lip coverage is present, plaque and gingivitis are likely to be more severe.13
The effects of oral breathing go beyond dental health. As the Norwegian orthodontist Dr. Egil Harvold discovered in his experiments on monkeys, mouth breathing during childhood causes irreversible changes to facial growth.14 It negatively affects the development of the nasal airway,15 potentially leading to a lifetime of breathing and associated health problems. These include cardiovascular disorders, sleep disorders, physical pain, and even sexual dysfunction. Oral breathing plays a role in speech disorders,16 postural changes,17 and sleep-disordered breathing that can result in cognitive impairment in children.18 Children with obstructive sleep apnea typically display swollen adenoids and tonsils, malocclusion, and craniofacial abnormalities,9 which further increase the risk of dry mouth and mouth breathing. There is a relationship between oral breathing, atopic dermatitis, and tonsillitis.20 Mouth breathers also experience behavioral changes, including poor concentration, daytime sleepiness, anxiety, restlessness, and bad moods.1
Simple steps to identify oral breathing in your patients
One of the problems facing dentists is that oral breathing can be difficult to diagnose, especially if the nose is not physically blocked.
In one survey of orthodontists in Brazil, the main diagnostic criteria for oral breathing were body posture (97.8%), lip competence (96.7%), and dark circles under the eyes (86.7%). The interviewees associated disease most strongly with the duration of mouth breathing.1 Patients who had breathed orally for longer showed more obvious symptoms.
There are certain markers that can help differentiate between habit and organic obstruction. Pacheco, et al., suggest detailed clinical guidelines for the identification of mouth breathing in children.21 The same procedure can be followed with adults.
With the patient seated, look for the following:
- Dark eye circles
- Postural changes such as a forward head thrust
- A long face (often with a recessed chin and a bent nose)
With the patient standing, look for the following:
- A high narrow palate
- Gingivitis in the maxillary incisors
- Anterior open bite
You can ask the patient (or the parent on the child’s behalf):
- Do you snore?
- Do you awake with a dry mouth in the morning?
- Do you drool on your pillow?
- Do you awake with a headache?
- Do you toss and turn during the night or wet the bed?
- Are you frequently tired during the day?
- Do you often have a stuffy, runny, or blocked nose, and/or runny nose?
- Do you often have allergies?
- Is it hard for you to concentrate?
- Do you struggle at work/school?21
New research identifies the presence of an atypical swallowing habit as the key link between habits that promote dental malocclusion of the vertical, transverse, and sagittal planes.7 Atypical swallowing suggests poor tongue function and is related to oral breathing. When the mouth is open, the normal resting position of the tongue is compromised. Over time, this affects function and strength in the tongue muscles.
You can also perform breathing tests to identify mouth breathing in your patients. The lip seal test in which the patient’s mouth is sealed with medical tape for 3 minutes4,21 has been proven to provide an objective screening tool. It allows the orthodontist to identify whether mouth breathing is caused by physical nasal obstruction or habit. Around 93% of people will be able to breathe through the nose. Even among habitual mouth breathers, more than 83% can breathe nasally for 3 minutes.4
What causes mouth breathing to persist?
Chronic mouth breathing often starts as the result of nasal obstruction that blocks the airway and makes nose breathing uncomfortable. In newborn babies, nasal obstruction is very rare.22 But during childhood, swollen adenoids and/or tonsils, or other conditions that block the nose22 prompt oral breathing. Around 40% of children in the United States have allergic rhinitis.22 In adults, as many as 63% have some type of rhinitis.23 Mouth breathing may also be caused by a deviated nasal septum, cleft palate, or a tongue-tie or lip-tie that make breastfeeding difficult. Tongue-tie may also cause abnormal swallowing, which as we’ve seen, is a risk factor for dental problems.7
The initial cause of mouth breathing may be physical obstruction or anatomical predisposition. But it is not enough to simply decongest the nose, remove the adenoids/tonsils, or perform turbinate reduction surgery. It is vital that mouth breathing behavior is changed. In most cases, after mechanical factors are removed, mouth breathing continues because it has become habitual.1 Mouth breathing can itself be the cause of nasal stuffiness, and so it becomes a self-perpetuating problem. It is essential, therefore, to retrain the breathing to prevent the problem recurring.
In 1994, I had turbinate reduction surgery to alleviate years of chronic nasal congestion. After surgery, there was no instruction to breathe through my nose. I continued to have sleep disorders for several years until I read an article about the importance of nasal breathing. My experience is far from unique. Dr. Christian Guilleminault, who is considered a founding father of sleep medicine, reported that the persistence of mouth breathing after adenotonsillectomy contributes to progressive worsening of sleep apnea. This frequently occurs within 3 years of surgery.24 Mouth breathing during sleep causes increased apneas and hypopneas, and worse oxygen desaturation.25 Dr. Guilleminault stated that successful treatment of pediatric obstructive sleep apnea and sleep-disordered breathing depends on the restoration of continuous nasal breathing during wakefulness and sleep.24 Without this vital step, surgery is a short-term fix.
The nasal obstruction that causes oral breathing can be addressed using breathing exercises to reduce the speed and volume of the breath and restore full-time nasal breathing. Rhinitis, for instance, which is the most frequent cause of nasal congestion, can be significantly reduced with this type of breathing retraining.26 Despite Dr. Guilleminault’s research, I am aware of very few ENT specialists who offer a nasal breathing program to support full recovery post-surgery.
Simple steps to help resolve oral breathing
Breathing re-education involves simple exercises designed to decongest the nose and restore normal breathing patterns. By showing children and adults how to decongest the nose, the dentist can help remove the feeling of air hunger that accompanies nasal congestion. Practice of specific breathing patterns optimizes breathing. This makes it comfortable and effortless for the child or adult to breathe through the nose.
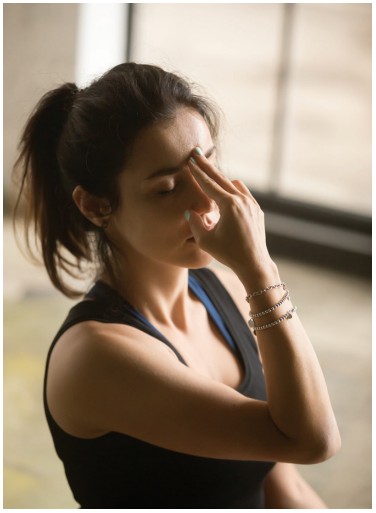
To ensure nasal breathing during sleep, it is necessary to tape the mouth with a specialist lip tape or a medical paper tape such as lip seal, 3M™ Micropore™ Surgical Tape, or MyoTape™. MyoTape is my own product. It is designed to be different from other lip tapes. The tape does not cover the mouth, meaning it is still possible to open the mouth to breathe if necessary. This is essential if using lip tape with a child or a patient who is fearful of suffocation.
Children aged 5 years and older can be encouraged to wear MyoTape for 15 to 30 minutes a day during rest. This works well when the child is distracted — playing, watching TV, or using a tablet. MyoTape is elasticated and gently brings the lips together. When the child opens the mouth to breathe, the tape gently reminds the child to breathe only through the nose. This helps change the mouth breathing behavior.
An exercise to decongest the nose
This exercise can be used any time the nose becomes blocked. To achieve long-term results, it should be followed with regular practice of breathing exercises to restore functional, nasal breathing. (Please don’t practice if you are pregnant, have sleep apnea, or have serious medical conditions.)
- Take a silent breath in through your nose if you can. If you can’t breathe in through your nose, take a small sip of air in through the corner of your mouth.
- Release a silent breath out through your nose (or the corner of your mouth).
- After the exhalation, pinch your nose to hold your breath. Keep your mouth closed.
- With your breath held, gently nod your head, or sway your body from side to side.
- Do this until you feel you cannot hold your breath any longer. You will feel quite a strong “hunger” or need for
- Let go of your nose, and breathe gently in through it. Keep your mouth closed, and avoid taking a large breath. Calm your breathing by focusing on relaxation.
- If your nose is still blocked, wait around a minute, and repeat the exercise.
- You may need to do the exercises several times before your nose is completely clear.
You can test the difference in airflow before and after the exercise by performing a “fog” test using your smartphone screen or a small mirror.
You will find a version of this exercise for children on the ButeykoClinic app, which is available on android and iTunes. The app features a complete program of children’s breathing exercises, free of charge.
The role of the dentist
Mouth breathing in children and adults is not innocuous. It has major implications for craniofacial development in children, and it contributes to gum disease, dental cavities, and bad breath — all problems the dentist works to resolve. To ensure a better service with the best long-term outcome for patients, it is imperative that dentists advise their pediatric and adult patients to breathe through the nose during rest, sleep, and exercise.
For more information on correct oral breathing, read “Lifetime effects of mouth breathing” by Michael Flanell at https://orthopracticeus.com/ce-articles/lifetime-effects-of-mouth-breathing/. Subscribers can take the quiz and receive 2 CE credits!
References
- Menezes VA, Cavalcanti LL, Albuquerque TC, Garcia AFG, Leal RB. Mouth breathing within a multidisciplinary approach: Perception of orthodontists in the city of Recife, Brazil. Dental Press J Orthod. 2011;16(6):84-92.
- Hitz Lindenmüller I, Lambrecht JT. Oral care. In: Surber C, Elsner P, Farage MA (eds). Current Problems in Dermatology. Vol 40. Karger Publishers; 2011.
- Carstensen S, Boyd K, Colquitt T, Cruz M, Raphael B. Promoting children’s oral health. J Am Dent Assoc. 2019;150(5):327.
- Zaghi S, Peterson C, Shamtoob S, et al. Assessment of nasal breathing using lip taping: a simple and effective screening tool. International Journal of Otorhinolaryngology. 2020;6(1):10.
- Abreu RR, Rocha RL, Guerra ÂFM. Prevalence of mouth breathing among children. J Pediatr (Rio J). 2008;84(5):467-70.
- Felcar JM, Bueno IR, Massan ACS, Torezan RP, Cardoso JR. Prevalência de respiradores bucais em crianças de idade escolar. [Prevalence of mouth breathing in children from an elementary school] [Article in Portuguese] Cien Saude Colet. 2010;15(2):437-444.
- Rodríguez-Olivos LHG, Chacón-Uscamaita PR, Quinto-Argote AG, Pumahualcca G, Pérez-Vargas LF. Deleterious oral habits related to vertical, transverse and sagittal dental malocclusion in pediatric patients. BMC Oral Health. 2022;22(1):88.
- Can a dry mouth cause cavities? [blog] Edwards Family Dentistry. https://www.westlittlerockdentist.com/can-a-dry-mouth-cause-cavities/. Accessed July 5, 2022.
- An overview of dry mouth. https://www.webmd.com/oral-health/guide/dental-health-dry-mouth. Accessed July 5, 2022.
- Su N, Marek CL, Ching V, Grushka M. Caries prevention for patients with dry mouth.J Can Dent Assoc. 2011;77:b85.
- Alqutami J, Elger W, Grafe N, et al. Dental health, halitosis and mouth breathing in 10-to-15 year old children: A potential connection. Eur J Paediatr Dent. 2019;20(4): 274-279.
- Pérez-González A, Suárez-Quintanilla JA, Otero-Rey E, et al. Association between xerostomia, oral and general health, and obesity in adults. A cross-sectional pilot study. Med Oral Patol Oral Cir Bucal. 2021;26(6):e762-e769.
- Gulati MS, Grewal N, Kaur A. A comparative study of effects of mouth breathing and normal breathing on gingival health in children. J Indian Soc Pedod Prev Dent. 1998; 16(3):72-83.
- Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981;79(4):359-372.
- Kalaskar R, Balasubramanian S, Kalaskar A. Correlation and comparative evaluation of nasal index and nasal cavity volume in nasal and mouth breathers: A preliminary cone-beam computed tomographic study.J Indian Soc Pedod Prev Dent. 2022;40(1):48-54.
- Hitos SF, Arakaki R, Solé D, Weckx LL. Oral breathing and speech disorders in children. J Pediatr (Rio J). 2013;89(4):361-365.
- T Neiva PD, Franco LP, Kirkwood RN, Becker HG. The effect of adenotonsillectomy on the position of head, cervical and thoracic spine and scapular girdle of mouth breathing children. International Journal of Pediatric Otorhinolaryngology. 2018;107:101-106.
- Boyd A, Golding J, Macleod J, et al. Cohort Profile: the ’children of the 90s’–the Index Offspring of The Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42(1):111-127.
- Tamasas B, Nelson T, Chen M. Oral health and oral health-related quality of life in children with obstructive sleep apnea. J Clin Sleep Med. 2019;15(3):445-452.
- Lee DW, Kim JG, Yang YM. Influence of mouth breathing on atopic dermatitis risk and oral health in children: A population-based cross-sectional study. J Dent Sci. 2021; 16(1):178-185.
- Pacheco MCT, Casagrande CF, Teixeira LP, Finck NS, Araújo MTM de. Guidelines proposal for clinical recognition of mouth breathing children. Dental Press J Orthod. 2015;20(4):39-44.
- Trabalon M, Schaal B. It takes a mouth to eat and a nose to breathe: abnormal oral respiration affects neonates’ oral competence and systemic adaptation. Int J Pediatr. 2012;2012:207605.
- Savouré M, Bousquet J, Jaakkola JJK, et al. Worldwide prevalence of rhinitis in adults: A review of definitions and temporal evolution. Clin Transl Allergy. 2022;12(3):e12130.
- Lee SY, Guilleminault C, Chiu HY, Sullivan SS. Mouth breathing, “nasal disuse,” and pediatric sleep-disordered breathing. Sleep Breath. 2015;19(4):1257-1264.
- Hsu YB, Lan MY, Huang YC, Kao MC, Lan MC. Association between breathing route, oxygen desaturation, and upper airway morphology. 2021;131(2): E659-E664.
- Adelola OA, Oosthuizen JC, Oosthuiven JC, Fenton JE. Role of Buteyko breathing technique in asthmatics with nasal symptoms. Clin Otolaryngol. 2013;38(2):190-191.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Patrick McKeown for the past 20 years has provided functional breathing training for children and adults to decongest the nose and restore nasal breathing during rest, exercise, and sleep. He is fellow of the Royal Society of Biology in the UK, founder of Buteyko Clinic International, and creator of the Oxygen Advantage® method. Patrick McKeown is the founder of MyoTape™ — the only lip tape that goes around the mouth instead of sealing the lips.
Patrick McKeown for the past 20 years has provided functional breathing training for children and adults to decongest the nose and restore nasal breathing during rest, exercise, and sleep. He is fellow of the Royal Society of Biology in the UK, founder of Buteyko Clinic International, and creator of the Oxygen Advantage® method. Patrick McKeown is the founder of MyoTape™ — the only lip tape that goes around the mouth instead of sealing the lips.
