Dr. Duane Grummons illustrates Grummons Facemask therapy and outlines its benefits.
Dr. Duane Grummons discusses the benefits of Facemask therapy
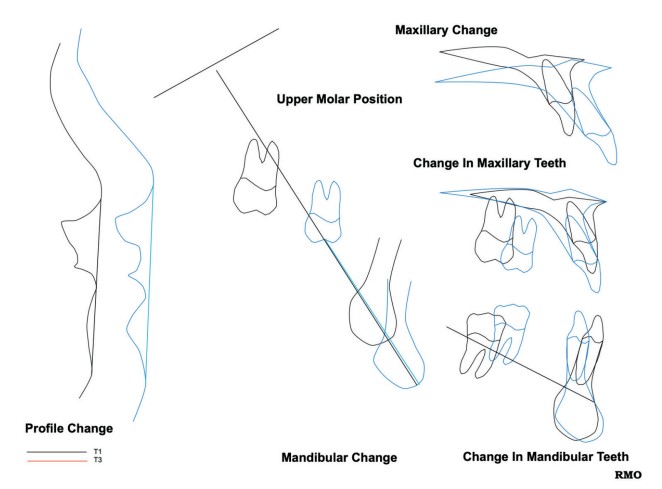
Nasomaxillary respiratory orthopedic applications of the Grummons Facemask with individualized protraction and slow palatal expansion show validated sutural responses and favorable airway flow benefits. Resolution is achieved with transverse and protraction movements of maxillae with circummaxillary sutural growth modification.1 Favorable effects follow:
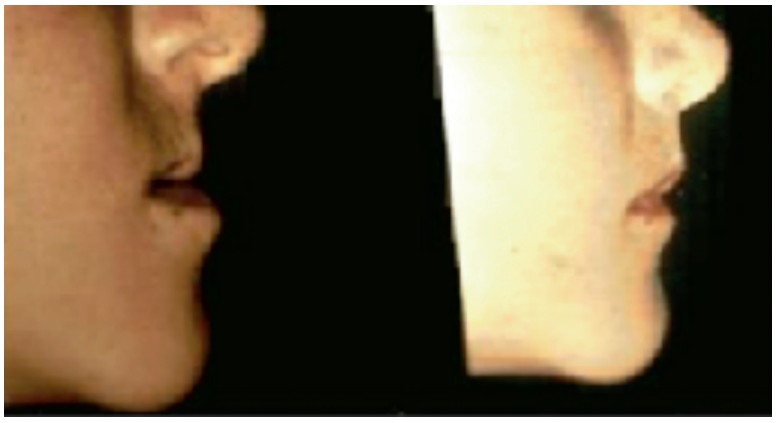
- more convexity of facial profile with forward relocation of maxillae
- proclination of maxillary incisors
- counterclockwise rotation of palatal plane2
- neutral posturing of mandible
- clockwise rotation of mandibular plane
- more upright lower incisors
- improved airway width and flow characteristics

Skeletal Class III patients have maxillary deficiency in 85% of cases; mandibular excess in 5% to 8%; combination in 7% to 10%.3 Airway and breathing disordered sleep (SDB) are priorities. Maxillae articulate through the following:
- midpalatal (MPS)
- frontomaxillary (FMS)
- zygomaticomaxillary sutures (ZMS)
- transverse palatine (TPS)
- nasomaxillary
- lacrimal

Zygoma (malar) and external orbital regions are divinely designed to mature early to protect orbital vital structures. ZM sutural configurations are obliquely oriented, tortuous, and intermingled to withstand trauma and sustained compressive loading of the facemask. Maxillary complex research used lateral implants from 4 to 21 years.4 Superimpositions of zygomatic processes proved no striking remodeling of the anterior surface in the anteroposterior direction.5 Malar stability permits facemask pads to rest here.

ZM sutures are resistive to remodeling.6 Complexity of interdigitations is greater in ZMS than other circummaxillary sutures. ZMS are longest and thickest of maxillary sutures, which limits change under protraction forces. When mid-palatal and nearby sutures are orthopedically activated, the ZM suture does not respond in the same ways.Serial x-rays of children’s zygomatic/malar relationships and point A were reported.7 After these studies, the Grummons Facemask with frontal/zygoma support was innovated.
Earlier intervention
Facial growth is 60% completed by ages 5 to 6 and 80% by age 8. Earlier treatment involves a nasomaxillary orthopedic expander, facemask protraction therapy, a mandibular dentoalveolar expander, and occlusal composites on primary molars bilaterally. As primary posterior teeth expand, the alveolar processes remodel wider with increased arch perimeter for unerupted teeth and area for tongue volume away from pharyngeal region. Myofunctional therapy (MFT) corrects low tongue posture, abnormal swallow, and helps achieve nasal breathing.
Facial orthopedics or surgery overcome Class III underbite and midfacial mismatches. Transverse sutural and alveolar remodeling occur with forward displacement of the maxillary complex from the pterygoid region. Facemask therapy in primary dentition is 70% orthopedics and 30% dentoalveolar; mixed dentition is 30% orthopedics, 70% dentoalveolar; and permanent dentition is dentoalveolar.

Facemask shaping is individualized:
- Facemask bendable to facial
- Bend malar supports by knuckle of finger to create malar contour.
- Frontal support above eyebrows.
- Bend frame longer, shorter, wider, or narrower to match face.
- Place pads on frontal and malar regions; extra pads for comfort.
- Place passively. If crib is on lips, add one to three pads on malar supports so crib clears lips.
- Velcro headstrap to frame with light fit to occipital region.
- Place facemask from behind into place in one motion.
- Readjust headstrap so mask is oriented to face and comfortable.
- Elastics from molar band hooks or from buccal arms to crib. Traction is forward and downward.
- Protocol: bilateral 3/8 or 5/16 inch, 8 oz. elastics for first 1 to 2 weeks; transition to ¼ or ½ inch, 6.5 oz. heavy, or 5/16 or ½ in 14 oz. elastics.
- Begin 1 to 2 hours wear while awake; soon while sleeping 8 to 10 hours.
- Optimum: 8 to 10 hours traction for maxillary orthopedics forward.

Week 1: Facemask, 1 hour awake; one elastic per side
Week 2: Two hours awake; two elastics per side
Week 3: One hour before bedtime and while sleeping, two elastics per side
Midfacial orthopedics with transverse maxillae expansion can be skeletal (sutural), dentoalveolar, and/or dental arch. Thin-plate spline analysis of rapid maxillary expansion with facemask therapy in early Class III malocclusions shows forward displacement of the maxillary complex from pterygoid region with clockwise rotation of mandible.8 Nasomaxillary respiratory regions are better developed with protraction facemask therapy and orthopedic SLOW expansion of 2 to 3 turns per week.

Point A is most anterior point in convexity of maxillae in median sagittal plane. Well-balanced adult faces have point A ahead of nasion perpendicular by 4 mm in females and 1.1 mm in males, reported by McNamara.9 Maino G, et al.,10 Ricketts and Grummons11 recommended forward placement of point A with convexity of +3-4mm (face forward).

Facemask and slow PE/ME
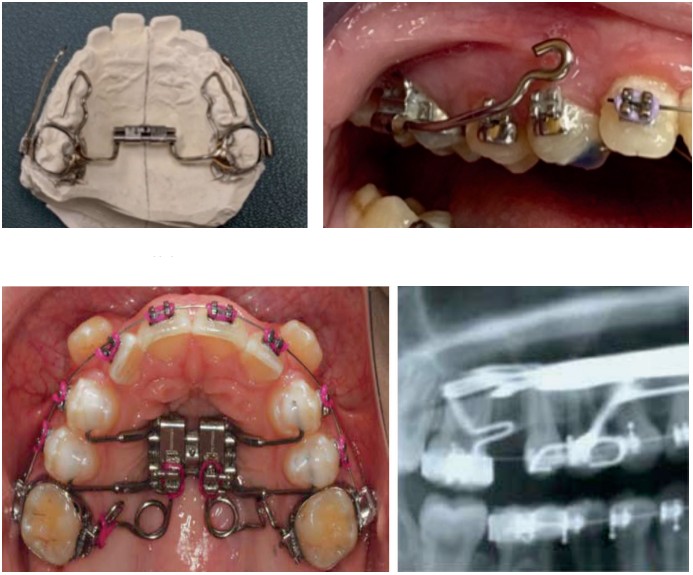
Facemask protraction of the nasomaxillary complex with point A relocation forward is a key clinical objective. The maxillary expander has bilateral buccal arms soldered to molar bands, extending forward to the region of maxillary canines. Slow activations best influence the circummaxillary sutures and nasomaxillary respiratory regions.

Typically, maxillary skeletal deficiency patients demonstrate mandibular over-closure with lower facial vertical deficiency. Occlusal molar composites lift the bite.
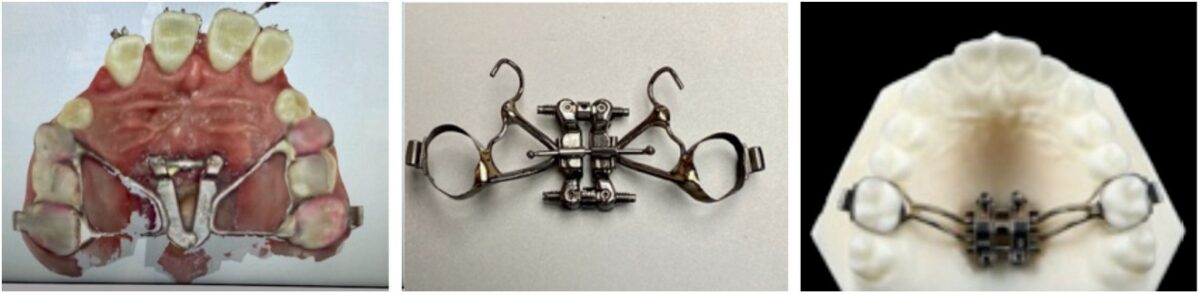
The 3-Way maxillae expander12 with molar springs provides derotation as maxillae-palatine structures are protracted with the Grummons orthopedic Facemask. Movements are three-dimensional (tip, yaw, roll): molar extrusion/intrusion, occlusal plane leveling, and midline correction.
BAMP (bone-anchored maxillary protraction) RPE or MSE (Moon) palatal expander (MARPE) with facemask yields greater maxillary advancement compared to facemask with tooth-borne maxillary expansion.
Maxillary midline (yaw) correction is achieved with buccal arms shorter on one side, so the dental arch moves forward and midline improves by shifting to opposite side. Buccal arms are adjusted parallel to the occlusal plane (OP) for straight pull forward. One buccal arm can be bent higher at the canine region, so the dental arch moves inferiorly as occlusal plane levels (roll). Mandibular protraction of both arches corrects bidental retrusion. The upper arch can move forward in Class III malocclusion. Elastics from lower molars to facemask crib relocate the lower arch forward to help correct Class II malocclusion to the extent periodontal support permits.

Research on the Grummons Facemask13 showed decisive improvements in the sagittal-basal relations as upper molars moved forward 4.1 mm from pterygoid vertical with point A moved 2.2 mm forward. Grummons Facemask relocated maxillary point A forward by 3.4 mm for the composite sample.14 The effectiveness of alternating expansion and constriction enhances maxillary protraction.
Surgically facilitated orthodontic treatment (SFOT) (premolars previously removed by colleague’s treatment) included a palatal expansion appliance with bilateral corticotomies (maxillae surgically mobilized), and TADS with facemask protraction.
Sustained TMJ compression is un-favorable to the TMJ components that are designed for intermittent loading during functional movements. A facemask with chin-cup delivers unfavorable compressive loading upon TMJ posterior attachment, collateral ligaments, and condyle-disc assembly. The chin-cup facemask caused 24% of TMJ internal derangements from forces that are non-physiologic and detrimental.15,16 Three types of protraction facemask headgear were researched17; the Grummons Facemask had no unfavorable TMJ effects.
Maxillary arch is template for lower
Facemask with elastics to the upper molars neutralizes the distal thrust of a Herbst or Class II corrector, so point A remains well-placed in the face. The perimeter and shape of maxillary arch influences lower arch dimensions (like a lid on a box). The lower arch has clinical limitations for arch expansion. The maxillary arch width is the template for mandibular arch width and lower arch emplacement. As the upper transverse is improved, the lower widens with decompensated and uprighted Curve of Wilson. As the lower teeth move/angulate forward, this adds to upper arch movement forward with facemask.
Upper airway dimensional changes improve laminar airflow following maxillary protraction upon craniofacial structures.18 Improvement was seen in sleep scores and symptoms after bimaxillary expansion with facemask protraction of arches forward.19
Summary
Treat earlier with Class III nasomaxillary respiratory corrective orthopedics with face-forward facemask changes. It is better to shape the child’s developing facial structures for best physiologic airway than to repair or manage them as adults. Let’s copy nature in her fundamental majesty.
After reading about Facemask therapy, see how Dr. Grummons’ naso-maxillary orthopedic 3-dimensional expander techniques can overcome structural form discrepancies of the maxillae:
https://orthopracticeus.com/ce-articles/3-way-maxillae-expander-appliance-innovations/
- Ngan PW, Hagg U, Yiu C, Wei SH. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod 1997;3(4):255-264.
- Angelieri F et al. Zygomaticomaxillary suture maturation: part II – the influence of sutural maturation on the response to maxillary protraction. Orthod Craniofac Res. 2017; 20(3):152-163.
- Grummons D. Nonextraction emphasis: space gaining efficiencies, part 1. World J Orthod. 2003;3:21-32,177-189.
- Bjork A, Skieller V. [Growth and development of maxillary complex.] [article in German] Inf Orthod Kieferorthop. 1984;16(1):9-52.
- Linge L. Tissue reactions in facial sutures subsequent to external mechanical influences; McNamara, JA: Monograph Number 6 Craniofacial Growth Series. 1976;256.
- Angelieri F, Franchi L, Cevidanes LHS, et al. Zygomaticomaxillary suture maturation: A predictor of maxillary protraction? Part I — a classification method. Orthod Craniofac Res. 2017;20(2):85-94.
- Petit HP. Adaptation following accelerated facial mask therapy. In: McNamara JA Jr, Ribbens KA, Howe RP (eds). Clinical alterations of the growing face. Monograph No. 14, Craniofacial Growth Series, Center for Human Growth and Development, University of Michigan, Ann Arbor; 1983.
- Baccetti T, McGill JS, Franchi L, McNamara JA Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113(3):333-343.
- McNamara JA Jr. An orthopedic approach to the treatment of Class III malocclusion in young patients. J Clin Orthod. 1997;21(9):598-608.
- Maino G, Turci Y, Arreghini A, et al. Skeletal and dentoalveolar effects of hybrid rapid palatal expansion and facemask treatment in growing skeletal Class III patients. Am J Orthod Dentofacial Orthop. 2018;153(2):262-268.
- Grummons D, Ricketts RM. Frontal cephalometrics: practical applications part 2. World J Orthod. 2004;5(2):99-119.
- Grummons D. 3-Way maxillae appliance innovations. Orthodontic Practice US. 2019;10(5):20-23.
- Hegmann M, Ruther AK. The Grummons facemask as an early treatment modality within a class III therapy concept. J Orofac Orthop. 2003;64(6):450-456.
- Beisiegel D. Masters Thesis; Loma Linda graduate school of orthodontics. 1994.
- Sugawara J, Mitani H. Facial growth of skeletal Class III malocclusion and the effects, limitations, and long-term dentofacial adaptations to chincap therapy. Semin Orthod. 1997;3(4):244-254.
- Grummons D. Orthodontics for the TMJ/TMD patient. Scottsdale, AZ: Wright & Company; 1994.
- Hakan El, Ciger S. Effects of 2 types of facemasks on condylar position. Am J Orthod Dentofacial Orthop. 2010;137(6):801-808.
- Gupta A. An evaluation of the sagittal upper airway dimension changes following treatment with maxillary protraction appliances. J of Contemporary Dentistry. 2011.
- Quo SD, Hyunh N, Guilleminault C. Transverse aspects of bimaxillary expansion therapy for pediatric sleep-disordered breathing. Sleep Med. 2017;30:45-51.
Stay Relevant With Orthodontic Practice US
Join our email list for CE courses and webinars, articles and mores

 Duane Grummons, DDS, MsD, ABO, is U.S. Board-certified in facial orthopedics and orthodontics. He has authored and lectured worldwide for 40 years regarding his facial frontal analysis, orthopedic Facemask and nonextraction appliance innovations. He is a leader in adolescent airway resolutions. Dr. Grummons is Associate Professor of Orthodontics at Loma Linda University Orthodontic Department in California. He developed two efficient and productive practices in Marina del Rey, California, and Spokane Washington. Dr. Grummons can be reached at grummons@me.com.
Duane Grummons, DDS, MsD, ABO, is U.S. Board-certified in facial orthopedics and orthodontics. He has authored and lectured worldwide for 40 years regarding his facial frontal analysis, orthopedic Facemask and nonextraction appliance innovations. He is a leader in adolescent airway resolutions. Dr. Grummons is Associate Professor of Orthodontics at Loma Linda University Orthodontic Department in California. He developed two efficient and productive practices in Marina del Rey, California, and Spokane Washington. Dr. Grummons can be reached at grummons@me.com.
